| R. Quesada, A. Moreno, I. Poves, E. Berjano, L. Grande, F. Burdío |
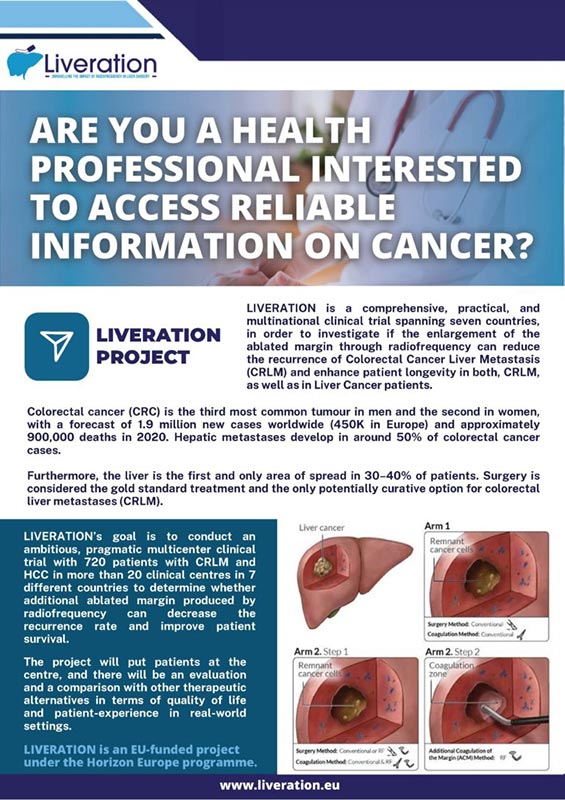
The impact of radiofrequency-assisted transection on local hepatic recurrence after resection of colorectal liver metastases |
Surgical Oncology |
2.017 |
26 |
229-235 |
https://www.sciencedirect.com/science/article/abs/pii/S0960740417300099?via%3Dihub |
|
| Villamonte, M., Burdío, F., Sánchez-Velázquez, P., Pérez, M., Martinez, A., & Ielpo, B |
New technique to increase resection margins during mini-invasive liver resection: a propensity score-matched study. |
Digestive Medicine Research (DMR) |
2.022 |
5 |
23 |
https://dmr.amegroups.org/article/view/8255/html |
|
| Villamonte, M., Burdío, F., Pueyo, E., Andaluz, A., Moll, X., Berjano, E., ... & Sánchez-Velázquez, P. |
The impact of additional margin coagulation with radiofrequency in liver resections with subcentimetric margin: can we improve the oncological results? A propensity score matching study. |
European Journal of Surgical Oncology |
2.022 |
48 |
82-88 |
https://www.sciencedirect.com/science/article/pii/S0748798321005709 |
|
| Ourania Koutsiouroumpa, Christos Christogiannis, & Dimitris Mavridis |
Introduction to meta-analysis and network meta analysis |
Video by University of Ioannina |
2.023 |
|
|
https://drive.google.com/file/d/1ZERtqGKC3sie20p_cqhqt6Beei7F_Ups/view |
|
| Christos Christogiannis, Ourania Koutsiouroumpa, & Dimitris Mavridis |
Introduction to survival analysis |
Video by University of Ioannina |
2.023 |
|
|
https://drive.google.com/file/d/1sqZv8_Lq8a9Jb2abqGRk9DMnPHxUtrCm/view |
|
| Yoshio Masuda, Mark Hao Xuan Yeo, Fernando Burdio, Patricia Sanchez-Velazquez, et al. |
Factors affecting overall survival and disease-free survival after surgery for hepatocellular carcinoma: a nomogram-based prognostic model—a Western European multicenter study |
Updates in Surgery |
2.023 |
|
|
https://doi.org/10.1007/s13304-023-01656-8 |
|
| Antoniou, S.A., Mavridis, D., Tsokani, S. et al. |
Network meta-analysis as a tool in clinical practice guidelines. |
Surgical Endoscopy |
2.023 |
37 |
1-4 |
https://doi.org/10.1007/s00464-022-09772-z |
|
| G Seitidis, S Nikolakopoulos, EA Hennessy, EE Tanner-Smith & D Mavridis |
Network Meta-Analysis Techniques for Synthesizing Prevention Science Evidence |
Prevention Science |
2.022 |
23 |
415–424 |
https://doi.org/10.1007/s11121-021-01289-6 |
|
| Aaronson, N. K., Ahmedzai, S., Bergman, B., Bullinger, M., Cull, A., Duez, N. J., ... & Takeda, F. |
The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. |
JNCI: Journal of the National Cancer Institute |
1.993 |
85(5) |
365-376 |
https://doi.org/10.1093/jnci/85.5.365 |
FAD |
| Chie, W. C., Blazeby, J. M., Hsiao, C. F., Chiu, H. C., Poon, R. T., Mikoshiba, N., Al-Kadhimi, G., Heaton, N., Calara, J., Collins, P., Caddick, K., Costantini, A., Vilgrain, V., Trinquart, L., Chiang, C., & EORTC Quality of Life Group |
International cross-cultural field validation of an European Organization for Research and Treatment of Cancer questionnaire module for patients with primary liver cancer, the European Organization for Research and Treatment of Cancer quality-of-life questionnaire HCC18. |
Hepatology (Baltimore, Md.) |
2.012 |
55(4) |
1122–1129 |
https://doi.org/10.1002/hep.24798 |
FAD |
| Arditi, C., Eicher, M., Colomer‐Lahiguera, S., Bienvenu, C., Anchisi, S., Betticher, D., ... & Peytremann‐Bridevaux, I. |
Patients' experiences with cancer care in Switzerland: Results of a multicentre cross‐sectional survey. |
European Journal of Cancer Care |
2.022 |
31(6) |
e13705 |
https://doi.org/10.1111/ecc.13705 |
FAD |
| Evans, P., Schuurman, D., Stahlbrost, A., & Vervoort, K. (K. Malmberg, & I. Vaittinen, Ed.). |
Living Lab Methodology: Handbook. |
U4IoT Consortium |
2.017 |
|
|
DOI: 10.5281/zenodo.1146321. |
FAD |
| Kassianos, A.P (Ed.). |
Handbook of Quality of Life in Cancer |
Springer |
2.022 |
|
|
https://doi.org/10.1007/978-3-030-84702-9 |
FAD |